Treatment Options
- ClosureFast™ Radiofrequency Therapy
- Local anesthesia with no incisions or scarring
- Minimal pain, bruising, or swelling
- Immediate return to daily activities
- No need for tumescent anesthesia
- Only one needle stick
- No downtime or compression garments required
- Performed in short, multiple sessions
- Minimal discomfort, no scarring, and rare complications
- Compression dressing worn post-treatment
Why Choose VeinCare Expert?
- Expertise: Thousands of procedures performed by skilled physicians.
- Convenience: Most treatments are office-based with no downtime.
- Results: Exceptional cosmetic and functional outcomes.
Contact Us Today
General Principles
Your individualized treatment plan will be developed based upon your history, physical examination, diagnostic ultrasound results, response to conservative measures, and goals of therapy. Treatment is tailored to the individual’s anatomic and physiologic abnormalities. In general, the most prominent sources of high venous pressure, commonly the great and small saphenous veins, are addressed first.
Treatment of the more surface varicose veins follows. We treat from “biggest to smallest” and “inside to outside”. The truncal veins, if abnormal, are treated first, most commonly with office based endovenous radiofrequency or laser ablation. Remaining branches are then treated with a combination of sclerotherapy and/or microphlebectomy, all office based procedures.
Treatment of deep venous insufficiency, superficial and deep thrombophlebitis, congenital venous malformations, pelvic congestion syndromes, and other less common entities is highly individualized and should be discussed with your Northwest VeinCare physician.
Endovenous Thermal Ablation
ClosureFast™ Targeted Endovenous Therapy
EVLA (Endovenous Laser Ablation)
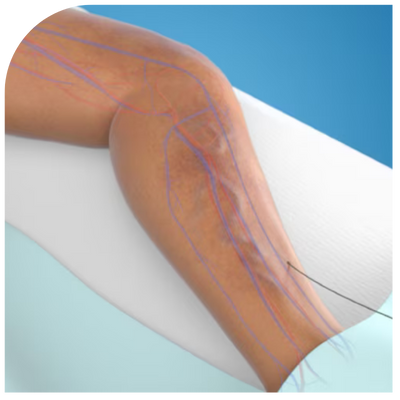
These minimally invasive procedures procedures are forms of endovenous thermal ablation, and are most commonly used to treat abnormal truncal veins of the lower extremity. Each applies heat in a controlled fashion to the inside of the diseased vein, using radiofrequency (RF) or laser as an energy source.
The targeted vein is sealed shut and, over time, is absorbed by the body. The procedures are similar in how they are performed. For RF, energy is transferred and heat applied by direct contact with the collagen of the vein wall. For laser, a specific wavelength of amplified light is used to target the water in the tissue of the vein wall. Using ultrasound guidance, your physician will position a catheter and treatment fiber into the diseased vein through a small puncture in the skin, similar to placing an IV catheter.
With the catheter in place, a solution is injected around the vein to provide local anesthesia and to prevent damage to surrounding tissues. Heat energy using laser or radiofrequency as a source is then precisely applied to the diseased vein using ultrasound guidance. After the targeted vein is closed, blood is redirected to other healthy veins to return to the heart. There are no incisions, no scarring, minimal or no pain, bruising, or swelling, and complications are extremely rare. Best of all, there is no down time. Normal daily activities may be resumed immediately.
Functional and cosmetic results are excellent, with the treated diseased vein remaining shut in approximately 95% of cases. The procedure is performed in the office and takes less than an hour. Your VeinCare physicians are amongst the most skilled and experienced in these procedures, having performed thousands in a comfortable and convenient office setting.
Venaseal (Cyanoacrylate Ablation)
Venaseal is a non-thermal ablation procedure used to treat the truncal veins of the lower extremity. Tumescent local anesthesia is unnecessary so there is only one needle stick (at the catheter insertion site). Small dabs of cyanoacrylate medical adhesive are injected while pressure is applied over the vein.
There is no down time and no need to wear compression afterward. The procedure is very effective, with results similar to thermal ablation. Your Veincare Experts physicians are skilled and experienced in this procedure and were amongst the first in the Chicagoland area to perform Venaseal ablation.
Sclerotherapy (Endovenous Chemical Ablation)
After truncal veins are satisfactorily addressed, or if they are not an issue, then branches or tributaries are treated, most commonly with sclerotherapy. An FDA approved sclerosing agent is injected into the vein, destroying its lining and prompting the vein to close shut.
Sodium Tetradecyl Sulfate or Polidocanol are commonly used, either as a liquid or a foam. As with the truncal veins, blood is routed to more efficient routes. Unlike treatment of truncal veins, sclerotherapy for tributaries usually requires a series of shorter appointments. At each session, several injections are performed at key locations using a very small needle. The injection is guided by direct vision, palpation, or by duplex ultrasound imaging.
A compression dressing is worn for several days afterwards. Sclerotherapy has also been used for truncal veins, but more effective treatments are usually used today. Sclerotherapy is also used for spider veins, and is very efficient, although other modalities are available. Treatments are virtually painless except for tiny needle sticks, there is no scarring, complications are extremely rare, and there is no down time. Your Northwest VeinCare physicians have performed these treatments countless times with excellent cosmetic and functional results.
Ambulatory Microphlebectomy (Stab-Avulsion Phlebectomy)
In this procedure, veins are actually removed, but unlike conventional stripping, tiny (1-3 mm) punctures are made with a fine scalpel or needle tip and the diseased veins removed using tumescent anesthesia and a special hook shaped dissecting instrument. The configuration and location of diseased veins determines when this procedure may be recommended.
The procedure may be performed in the office or out patient operating room, depending on how extensive the diseased veins are. Scars are tiny, there is minimal pain, and no down time. Dr. Robin is expert at this procedure and has performed several hundred.
Surgical Stripping
Conventional surgical stripping, has, for the most part, been abandoned in favor of less invasive procedures.
Subfascial Endoscpic Perforator Surgery
This minimally invasive videoscopic procedure allows the surgeon to divide abnormal perforator veins in the lower leg. The videoscope and dissecting instruments are inserted through very small incisions just below the knee. It is performed in the operating room using regional or general anesthesia, and is usually reserved for patients with severe skin changes or ulcers.
Dr. Robin was one of the first in the Chicago area to perform this procedure. It is used infrequently today since perforator veins can now be addressed by even less invasive percutaneous laser, radiofrequency, or sclerotherapy procedures.